- Your skin
-
Our products
Do you know well atopic dermatitis ?
DEXERYL supports you and take care of your dry skin each day
-
CLINICAL RESULTS
- About dexeryl

Atopic dermatitis, also known as atopic eczema is a chronic inflammatory skin condition. But what is atopic eczema? What are the symptoms? What are the causes? How can you tell it apart from other types of eczema? What can be done to alleviate it and space out the flare-ups?

Summary
of the population in Europe is affected
of children suffer from atopic dermatitis
is the risk of a child being affected if both parents have atopic dermatitis
Atopic eczema is a chronic inflammatory skin condition (hence its other name, dermatitis), which develops in flare-ups, i.e. alternating between remission and symptomatic phases2. These phases vary in duration.
Atopy occurs when there is a hereditary predisposition to develop symptoms of immediate hypersensitivity, such as hay fever, asthma, etc.3
Studies have shown that 50-70% of people with atopic dermatitis have a first-degree relative (father, mother, brother or sister) who also suffers from it1. Furthermore, if both parents are affected, the risk of the child developing atopic eczema increases to 80%4.
Atopic eczema affects mostly children. It most often appears from the age of 3 months onwards, and is therefore known as infant eczema. It develops in flare-ups during childhood and usually disappears in adolescence. However, it may persist into adulthood.



Scratchin lesions due to atopic eczema can sometimes become infected with bacteria (staphylococcus) or viruses (herpes). It is, therefore, essential that a doctor is consulted if there are changes in the appearance of the eczema patches, especially if they are accompanied by pain, fever and/or a change in general condition1.
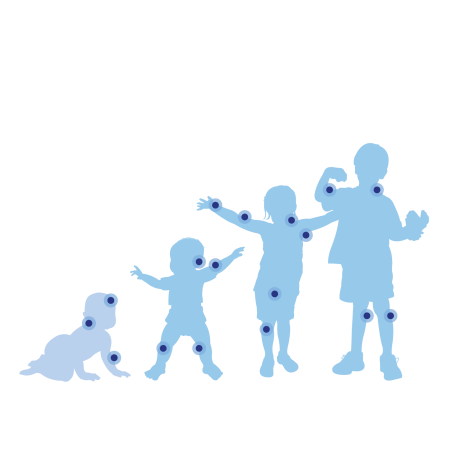
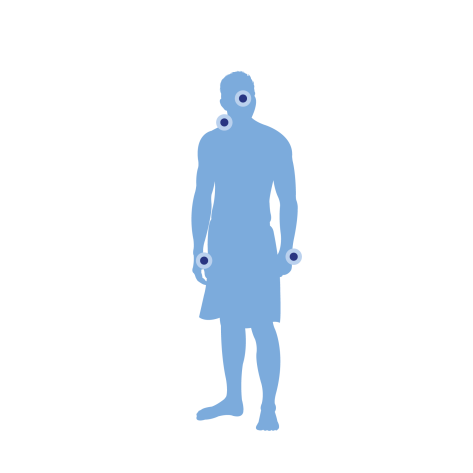
The lesions of atopic eczema are found on characteristic areas of the body, which evolve with age5



Atopic eczema is the consequence of a range of immunological and skin dysfunctions.
A person suffering from atopic eczema has an altered skin barrier characterised by a reduction of the natural protective hydrolipidic film. The skin can therefore no longer fulfil its barrier function, which makes it more sensitive to external aggressors. Environmental molecules called allergens such as pollen, dust, etc. can, therefore, penetrate the skin more easily and come into contact with the skin's immune cells. This triggers an inflammatory, maladaptive response that causes the symptoms of eczema. This lack of hydrolipidic film is also accompanied by significant skin dryness1.
In addition to having skin that is more permeable to allergens, people with atopic dermatitis also secrete high amounts of antibodies called IgE or immunoglobulin type E. This is a specific immune system response to the presence of allergens. This high level of IgE causes the body to overreact to the allergen aggressor1,3.
Over the past 30 years, there has been a significant increase in the number of cases of atopic dermatitis in developed countries.
Changes in infant feeding, particularly the decline in breastfeeding during the first three months of life and earlier dietary diversification, may partly explain this phenomenon4.
Another hypothesis put forward by scientists to try to explain this increase is that the more hygienic environment of infants and young children may reduce and delay the exposure of their immune system to a wide variety of substances, making it more sensitive4. This so-called hygiene hypothesis could also be the cause of other allergic manifestations.
Local treatment of atopic eczema is symptomatic, i.e. it relieves symptoms such as itching and patches without making the condition disappear permanently. It also helps to limit the occurrence of new flare-ups and, therefore, also to space out the flare-ups7.
The treatment is prescribed by a doctor (usually a general practitioner, paediatrician or dermatologist) after a clinical examination and diagnosis of atopic dermatitis. It is essentially based on the application of corticosteroids (cortisone cream or ointment) to the lesions until they disappear. This takes an average of one to three weeks. The strength of the corticosteroid and its dosage should be determined by the doctor.
If the corticosteroid fails, a local immunomodulator can be prescribed, i.e. a drug that will decrease the immune response on the skin, where the drug is applied.
UVA and UVB phototherapy can also be used by a dermatologist. This involves repeated skin exposure to lamps emitting UVA or UVB radiation. In the case of UVA, exposure is preceded by psoralen (often taken orally). It is a photosensitising compound that is supposed to make the skin more sensitive to UV radiation. It is effective in the short term but must be used in moderation.
Finally, when local treatments are not sufficient, systemic treatments (oral or injectable) can be considered. These include immunosuppressants and biotherapy drugs that act on the patient's immune system to reduce atopic symptoms8,9.
Finally, investigating the responsible allergens may be considered, especially if a correctly performed local treatment has failed.
In addition to the medical management of atopic eczema, it is important to adopt a specific routine to take care of your skin every day.
Atopic eczema requires long-term management: simple measures implemented every day can improve the effectiveness of treatments, space out flare-ups and improve patients' quality of life1.
People with atopic eczema have permanently dry skin all over the body, which impairs the barrier function of the epidermis. The use of emollient, i.e. moisturising, creams helps to restore this function. Emollients should be applied all over the body, once or twice a day. Regular application of emollients helps to space and minimise flare-ups and reduce the use of corticosteroids.
Daily application of an emollient helps to space out flare-ups and reduce the use of corticosteroids. Proper daily moisturising and hygiene will work in synergy.
Our expert
" Like European experts, I recommend the use of emollients as a background treatment to prevent flare-ups of atopic dermatitis "*
*Wollenberg A. et al. European guideline (EuroGuiDerm) on atopic eczema. JEADV. Volume 36, Sep 2022. 1409-1431. e
flare-ups of atopic dermatitis¹
skin dryness²
fewer patients used corticosteroids¹
The basis for treating xerosis is, above all, moisturising the skin and appropriate hygiene.
DEXERYL supports you with emollient skin care and cleansers specially formulated for sensitive skin and recommended for the treatment of signs of skin dryness (xerosis).

DEXERYL Emollient Cream can be used to protect the skin and treat the signs and symptoms of dry skin, particularly in the context of atopic dermatitis, thanks to:
Discover the DEXERYL range
Sources: